Related article: Olmesartan (Benicar) and kidney disease

Table of Contents
Kidney (renal) function tests
Most patients on the MP experience temporary but well-defined increases in various markers of disease state and inflammation, consistent with an immunopathological response. Results of blood tests for kidney function can generate considerable angst for Marshall Protocol patients and their medical providers. Out of genuine concern for their patients, some physicians consider withholding prescription of olmesartan. Experiences on the MP show that this concern may be mostly unfounded. And that the aberrant test values are to be expected from the nature of the MP treatment.
Doctors may want to assess kidney function by testing creatinine clearance test or BUN and measure other indicators specific to each patient for a baseline and retest as appropriate. Due to immunopathology, lab these values may become temporarily abnormal until the inflammation resolves.
Measures of kidney function
- creatinine clearance (CrCl) – Measurement of the clearance of endogenous creatinine. The most valid test of kidney function. Compares the level of creatinine in urine with the creatinine level in the blood, usually based on measurements of a 24-hour urine sample and a blood sample drawn at the end of the 24-hour period
- creatinine – A break-down product of creatine phosphate in muscle, and is usually produced at a fairly constant rate by the body (depending on muscle mass).
- blood urea nitrogen (BUN) – A measure of the amount of nitrogen in the blood in the form of urea. urea is a substance secreted by the liver, and removed from the blood by the kidneys.
- glomerular filtration rate (GFR) – The volume of water filtered out of the plasma through glomerular capillary walls, which are located in the kidney. Best estimated by creatinine clearance test. The estimated value (eGFR) takes age, sex and race into account. Creatinine arising from ingested meat can raise blood levels to falsely lower eGFR.
Often MP patients will be told by their physicians they have a high BUN/creatinine ratio or high creatinine, which a physician may take to be an indication of kidney dysfunction. If this is concern, the physician may wish to order the creatinine clearance test, which is considered a more reliable indication of kidney function.
Olmesartan is renoprotective and has anti-inflammatory properties
Related article: Science behind olmesartan
Olmesartan has two key properties: Vitamin D Receptor agonistA substance such as olmesartan (Benicar) or 1,25-D which activates the Vitamin D Receptor and transcribes the genes necessary for a proper innate immune response. and potent anti-inflammatory. While it may seem logical to discontinue olmesartan given that it stimulates the immune response, leading to immunopathology and subsequently elevated kidney values, abruptly withdrawing olmesartan can be dangerous.
By reducing inflammation, olmesartan offers ongoing protection to the kidneys even while it is stimulating the VDR.1) 2) When the medication is discontinued, the patient's symptoms of disease can become significantly worse as olmesartan's anti-inflammatory protection is withdrawn. This is because while the drop in inflammation is immediate, the immune response which has been accelerated by olmesartan will continue to be strong even days, weeks, or months after discontinuing olmesartan.
Instead of discontinuing olmesartan, physicians are advised to work with their patients to employ one of several strategies to reduce the immunopathological response. Reducing, but not discontinuing entirely, antibiotics has often proven helpful.
If kidney values remain well above the acceptable range and olmesartan simply must be stopped, it is generally preferred to discontinue olmesartan gradually over the course of at least a couple weeks, and at any time except during an acute emergency.
The benefits of olmesartan on patients with kidney inflammation include:
- decreased insulin resistance, fewer symptoms of the metabolic syndrome, and decreased inflammation in patients with chronic kidney disease.3)
- the ability to ameliorate renal injury and fibrosis in rats when taken at ultrahigh doses.4)
- decreased (intra)renal vascular resistance, increased renal perfusion, and significantly reduced oxidative stress in patients with type 2 diabetes5)
- protection of the kidneys in diabetic nephropathy6)
- offer a survival benefit in hemodialysis patients, may help in preservation of renal function in predialysis patient, and affect the tissue repair process, reducing renal fibrosis7)
Recent studies of Olmesartan in patients
Increases in kidney metabolites on the Marshall Protocol
For MP patients with disease involvement in the kidneys, kidney-specific metabolites may increase in a way that is consistent with an active or activated immune response. The following research support this idea:
- BUN – One study found that hemodialysis patients who had high serum values of urea nitrogen (BUN) were less likely to have the acute infection, Helicobacter pylori.8) This suggests that temporary markers of kidney stress such as BUN may correlate with a robust and successful immune response.
- creatinine – According to Goldstein, clinicians caring for patients with acute kidney injury (AKI) have been hindered by the reliance on serum creatinine or decreased urine output, both kidney function markers, to make the AKI diagnosis. Even more vexing is the fact that similar serum creatinine changes can occur without kidney damage, for example in the context of dehydration, nephrotic syndrome or hepatorenal syndrome.9)
In a 2011 study appearing in Kidney International, Agarwal et al. gave 16 patients with chronic kidney disease daily doses of paricalcitol, an orally active vitamin D receptor (VDR) activator.10) (Note that the VDR plays a key role in innate immunityThe body's first line of defense against intracellular and other pathogens. According to the Marshall Pathogenesis the innate immune system becomes disabled as patients develop chronic disease..) The vitamin D analog was stopped after four days, and measurements were continued for three. During therapy, researchers found that subjects' serum creatinine significantly increased at a rate of 0.010 mg/dl/day and urine creatinine at a rate of 17.6 mg/day. Researchers also found a small increase in blood levels of BUN.
In conclusion, VDR activation may alter creatinine metabolism. An increase in creatinine generation may lead to an increase in serum creatinine and, if eGFR is used to measure kidney function, it may give the appearance that kidney function is declining when truly it may not be altered.
Rajiv Agarwal et al.11)
This work emphasizes the need for MP doctors to rely upon the 24-hour creatinine clearance test rather than eGFR to get the most accurate picture of real kidney function. Also, it validates the strategy of waiting-out abnormal creatinine values, rather than trying to intervene.
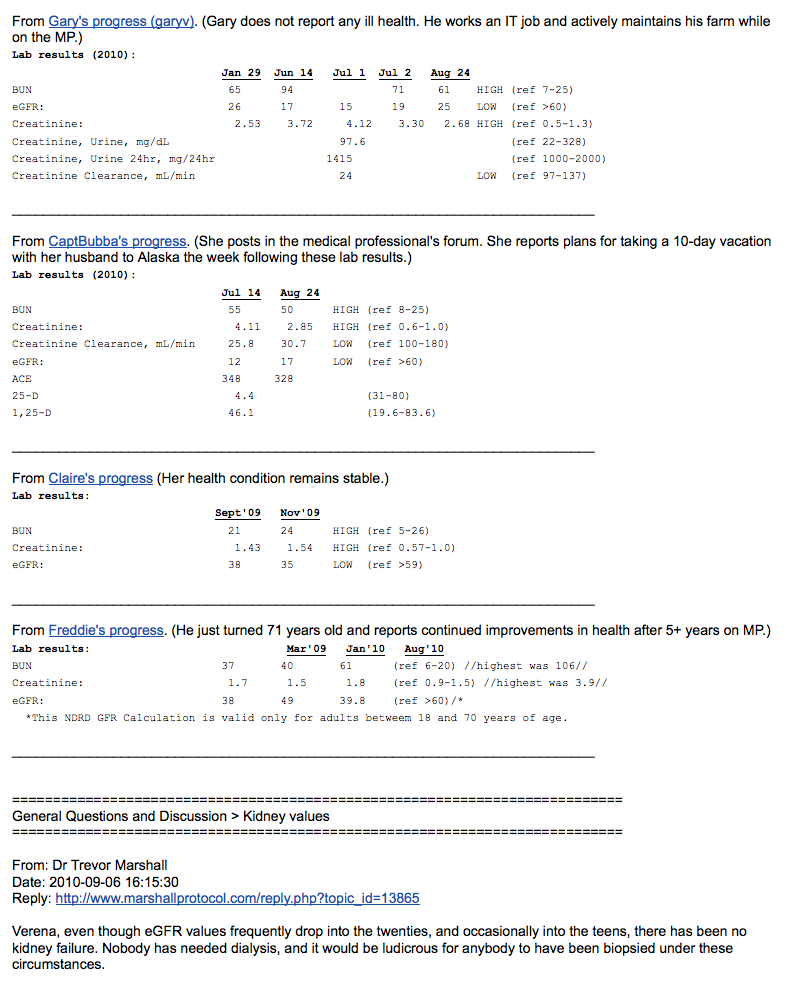
Patients experiences
As a matter of course, markers of kidney function including BUN and creatinine will fluctuate while a patient is on the MP. There is a tendency for some physicians to become alarmed by these fluctuations, particularly if a patient has kidney disease. However, for the vast majority of patients, these test results are an expected part of the healing process and will diminish over time.
Several patients have shown that measures of kidney function return to normal when they take measures (such as reducing antibiotics) to slow immunopathology.
I will have been off antibiotics for 25 days. My serum creatinine is now back down to 71 umol/L (0.81 mg/dL), with an eGFR of 80 mL/min. These are the same as before starting the MP, so my GP was “relieved” when I spoke to her this morning. I haven't been able to stop smiling all day!
Asilan, MarshallProtocol.com
Overall my health is mostly back to normal and I don’t notice any ill effects from these out of range kidney tests. However, as you can imagine, my Doc is quite alarmed. I have reviewed my 4 ½ year history with her (she is my third MP doc) and I have assured her that Benicar is renal protective, that it is normal for the kidneys to be loaded with toxins as the immune system eliminates the infection releasing toxins into the blood. And that this is proof, in fact, that the MP is working.
Measure Range 11/2007 4/2008 8/2008 9/2008 11/2008 4/2010 BUN (blood urea nitrogen) 7-25 24 30 (high) 32 (high) 18 40 (high) 35 (high) creatinine 0.5-1.3 1.3 1.2 1.59 (high) 1.23 1.54 (high) 1.57 (high) GFR (glomerular filtration rate) >60 44 (low) 59 45 (low) 44 (low) potassium 3.5-5.3 4.9 5 6.2 (high) 4.3 5.2 4.5 Gene Johnson, MarshallProtocol.com
Only Benicar every four hours during day time and a few times once at 3 a.m. My creatinine is down from 138 to 116 in a test taken two days ago (range 60-105). It was comforting to see that an increase in Benicar did not lead to an increase in creatinine as my nephrologist speculated it would.
Inge, MarshallProtocol.com
I received some good news during my doctor appointment. My kidney functioning tests were normal. My doctor had taken me off the MP meds back in May due to the increase in my creatinine and BUN. I wasn't sure how my tests results would be right now since I was now at the maximum doses of the MP meds. I was keeping my fingers crossed that the results would be good so my doctor wouldn't take me off the MP meds again. My doctor and I were both surprised to see that both my creatinine and BUN were normal.
Mike9a, MarshallProtocol.com
I'm now taking minocycline 25mg every two days Benicar 40mg every 3 to 5 hours. One week past “kidney crisis,” and new test results are almost normal. Whew.
Somadoc, MarshallProtocol.com
Comment
Creatinine level is an measure of activity, not a cause of damage (unlike v.D which is both a measure of, and cause of illness). Some researchers are considering its possible use as therapy
when used between 10–100 mM, suppression of growth and killing of all bacterial species were observed including not only drug-resistant strains, such as methicillin-resistant Staphylococcus aureus, but also uncharacterized environmental bacterial strains as well. The mechanism of action is as yet unclear.
Creatinine inhibits bacterial replication Thomas McDonald, Kristen M Drescher, Annika Weber and Steven Tracy 2012 12)
[PMID: 13679467] [DOI: 10.1093/ndt/gfg282]
[PMID: 16601581] [DOI: 10.1097/01.hjh.0000220413.22482.36]
[PMID: 17130263] [DOI: 10.1681/ASN.2006080916]
[PMID: 16755152] [DOI: 10.1291/hypres.29.169]
[PMID: 15716329] [DOI: 10.1681/ASN.2004100852]
[PMID: 20540037]
[PMID: 14696511]
[PMID: 22189039] [PMCID: 3287120] [DOI: 10.1186/1741-7015-9-135]
[PMID: 21716260] [DOI: 10.1038/ki.2011.207]
[PMID: 22293916] [DOI: 10.1038/ja.2011.131]
[PMID: 19074997] [PMCID: 2646021] [DOI: 10.2337/dc08-1265]